






Diabetic Retinopathy: Understanding the Vision Complications of Diabetes
Diabetes is a chronic disease that affects millions of people worldwide.
While most people know about the management of blood sugar levels and the potential complications such as
heart disease and kidney damage, one lesser-known consequence of diabetes is the development of diabetic
retinopathy.
What is Diabetic Retinopathy?
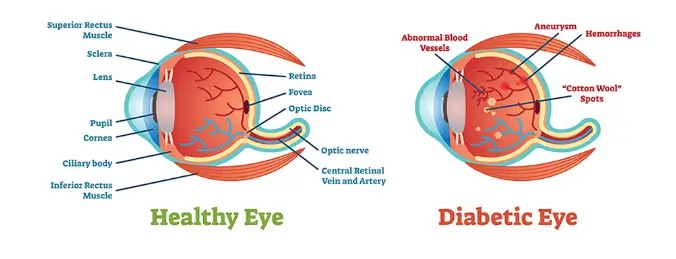
Diabetic retinopathy is a condition that occurs when high blood sugar levels damage the blood vessels in the retina,
the light-sensitive tissue at the back of the eye. Over time, these damaged blood vessels may leak or become blocked,
leading to vision disturbances or even vision loss.
The Stages of Diabetic Retinopathy:
1. Non-proliferative diabetic retinopathy (NPDR): In the early stage, small blood vessels in the retina begin to weaken and leak fluid. This can cause swelling in the macula, the central part of the retina responsible for detailed vision.
2. Proliferative diabetic retinopathy (PDR): In the more advanced stage, the body responds to the damaged blood vessels by growing new ones. However, these new blood vessels are fragile and can bleed into the vitreous gel, causing floaters and further vision loss.
How Does Diabetes Cause Retinopathy?
The exact mechanism by which diabetes leads to retinopathy is not fully understood. However, it is believed that prolonged exposure to high blood sugar levels damages the delicate blood vessels in the retina, impairing their ability to function properly.
Additionally, high blood pressure and high cholesterol, common coexisting conditions in individuals with diabetes, can further contribute to the progression of retinopathy
Reducing the Risk and Managing Diabetic Retinopathy: Prevention is key when it comes to diabetic retinopathy. Managing blood sugar levels, blood pressure, and cholesterol can help reduce the risk of developing the condition or slow its progression. Regular eye examinations are essential for individuals with diabetes, as early detection and intervention can prevent or minimize the vision loss associated with retinopathy. These exams typically involve dilating the pupils to allow for a detailed examination of the retina. In some cases, treatment options for diabetic retinopathy may include laser therapy, injections of medication into the eye, or surgery to remove scar tissue or blood from the retina.
Living with Diabetic Retinopathy:
For individuals already diagnosed with diabetic retinopathy,
there are steps that can be taken to maintain optimal eye health and preserve vision:
1. Control blood sugar levels: Keeping blood sugar levels within the target range set by a healthcare provider is crucial in minimizing the effects of retinopathy.
2. Monitor blood pressure and cholesterol: Managing these factors helps reduce the risk of further blood vessel damage.
3. Adopt a healthy lifestyle: Regular exercise, a balanced diet, and avoiding smoking can promote overall health, including eye health.
4. Regular eye examinations: These allow for timely intervention and treatment if necessary. Additionally, having a dialogue with an eye specialist can provide important information and guidance on managing the condition.
Conclusion:
Diabetic retinopathy is a serious complication of diabetes that can lead to vision loss if left untreated. Maintaining a proactive approach to diabetes management and regular eye examinations are essential in reducing the risk and impact of retinopathy.
By prioritizing the necessary lifestyle changes, individuals can take control of their eye health and work towards preserving their vision despite living with diabetes